 Abi Nardi
Abi Nardi
Licenciada en Fonoaudiología
Óptica contactóloga
Especialista en Audiología
Villa Dolores, Cordoba, Argentina
I am licensed to practice audiology and language therapy, a career path that takes 5 years to complete plus the final thesis in my country, Argentina. After graduating I dedicated myself to the area of audiology.
I have worked in a very prestigious hospital in a big city, and currently work in a smaller city, in a private practice and municipal clinics, knowing different social, emotional and economic realities, where each person goes through similar pathologies in different ways.
In my family I grew up learning to see the “patient” as a person first. My mother is an optometrist, and she always listened to her patients, showing me how to learn about each as persons first and what they contribute, before their pathologies.
However, in my years of the University I didn´t have, not even half a semester, a subject that taught me to LISTEN, CARE and ACCOMPANY a patient. Conversely I had the ones that taught me to carry out and understand tests, know pathologies and ways to solve them, from a purely scientific approach. I am obviously grateful because it is necessary to incorporate these topics and they are the basis of an audiologist’s college career.
But in my country it´s normal to attend patients within a certain time and try to unilaterally resolve the conditions — without remembering the environment, social, economic and emotional level of each person.
After gaining some experience, I needed to know a little more every day, to update me and learn. One day I found this website, got to know Kris English and through her the IDA Institute. I had been trying to provide patient-centered care for years in a disorganized way and without given it a name. I also had no coworkers interested in PCC, until now.
I Tell You What I Have Learned…
Person Centered Care (PCC) is a practice that is difficult to understand. It moves us from a structured job, or rather a traditional one, which is what we have been taught to exercise in a unidirectional way. I have learned that PCC proposes a more complex, dynamic professional exercise; we must be adaptable to what our patients are expressing and we must discover what they value. It means getting more involved in each consultation, paying extra attention to each situation that occurs in the meeting, managing to understand all aspects of our patient life.
There are situations that we cannot control, such as the culture where we live, that of our work, economic tools, our educational past, but nevertheless there many other situations that we can control.
I never spent hours explaining an audiogram, I have never been only theoretical; I always went further, observing whoever chose me as an audiologist, LISTENING to what he has to say, without asking closed questions, allowing freedom to express oneself. I know that it’s a unique experience each patient brings to their hearing loss, since for each one it means something different, having different thoughts, feelings and experiences according to how this loss is affecting him in his life.
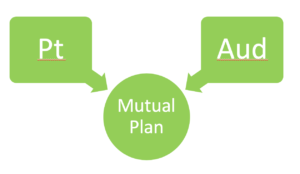
Recognizing that the way we interact with our patients has a significant effect in the auditory result means we see the importance of how to build a therapeutic relationship. And so we can position ourselves as clinicians, where we not only explain options, but we must also work with the goals and values of our patients, situating ourselves with EMPATHY. We help them chart a path with a plan appropriate to what we believe best for them, according to what they explicitly and implicitly propose to us in their narratives.
What Keeps Me Going…
I will never forget a patient who entered the consultation, referred by a colleague, who described him as a patient who didn’t accept his diagnosis: profound bilateral sensorineural hearing loss.
 We sat down… no one spoke for a minute, we just looked at each other, waiting for the other to speak…when suddenly he said to me: “ How comfortable I have felt for a moment, where nobody told me what to do or how, just waited for me to decide to speak…Now I´m going to tell you…”, Then I asked a few questions, since my patient described himself without questionnaires. And I asked myself: profound hearing loss? Without any testing? It turned out to be a patient with a wrong diagnosis.
We sat down… no one spoke for a minute, we just looked at each other, waiting for the other to speak…when suddenly he said to me: “ How comfortable I have felt for a moment, where nobody told me what to do or how, just waited for me to decide to speak…Now I´m going to tell you…”, Then I asked a few questions, since my patient described himself without questionnaires. And I asked myself: profound hearing loss? Without any testing? It turned out to be a patient with a wrong diagnosis.
That encounter occurred in 2019, and since then I have treated eight patients sent by him.
This is where, through PCC, I can fully appreciate what to do with this information and how to take advantage of it. Today I feel supported, accompanied, on track, I found academic training on the subject, I found those who gave it a “frame”
I Know that it’s in me and in every professional who wants it, the ability to respond to the emotions that derive from the hearing loss of our patients.
With these insights, I try to encourage colleagues to get involved and soak up this knowledge that is very simple to implement but complexly difficult to apply, especially if we don’t manage to deconstruct our way of looking the traditional clinician-patient relationship.
I understand the added value that we can achieve, but the structures of traditional education don’t put in value, hence it’s difficult to see and adopt it. The important thing is that if we manage to move from the traditional approach and adopt this way of working, we’ll quickly see that benefits are found for both parties: we manage to improve the patient’s health and we as professionals will have fidelity on their part. The idea of building loyalty to our patients, listening to them, making them feel at ease beyond getting involved in their problems and trying together to reach the best possible option for their condition. Simply by using the responsible practice of PCC.
Here is the future of our way of working effectively, responding to the global need of each person.

 Luego de saludarnos, nos sentamos… nadie habló por un minuto, solo nos miramos, esperando uno al otro para que hablara… cuando de repente me dijo: “qué a gusto me he sentido por un momento, donde nadie me dijo qué hacer ni cómo, solo me espero a que me decidiera a hablar… Ahora te voy a contar…”, luego realicé pocas preguntas, ya que mi paciente se describió solo sin necesidad de cuestionarios. Y me pregunté: ¿Hipoacusia profunda? Sin haberle realizado siquiera un estudio. Resulto ser un paciente con diagnóstico equivocado desde su narración hasta las pruebas realizadas posteriormente.
Luego de saludarnos, nos sentamos… nadie habló por un minuto, solo nos miramos, esperando uno al otro para que hablara… cuando de repente me dijo: “qué a gusto me he sentido por un momento, donde nadie me dijo qué hacer ni cómo, solo me espero a que me decidiera a hablar… Ahora te voy a contar…”, luego realicé pocas preguntas, ya que mi paciente se describió solo sin necesidad de cuestionarios. Y me pregunté: ¿Hipoacusia profunda? Sin haberle realizado siquiera un estudio. Resulto ser un paciente con diagnóstico equivocado desde su narración hasta las pruebas realizadas posteriormente.
 mind to find peace in the present moment. When we are truly listening, are we also not working to find peace within ourselves to be fully present for the person in front of us?
mind to find peace in the present moment. When we are truly listening, are we also not working to find peace within ourselves to be fully present for the person in front of us? recent being his daughter’s landmark birthday celebration. I let him talk. With tears in his eyes, he told me that he had sought an appointment at his GP for an assessment for dementia. My clinical ego wanted me to reassure him, and tell him everything is fine and to push on with the appointment. But instead, we sat and explored his concerns. We asked each other questions and we sat through conversation and silences that were uncomfortable for the both of us. We came to an agreement that we would get his hearing aids as good as they can be for his dementia assessment, so that we can face things confidently with our heads held high.
recent being his daughter’s landmark birthday celebration. I let him talk. With tears in his eyes, he told me that he had sought an appointment at his GP for an assessment for dementia. My clinical ego wanted me to reassure him, and tell him everything is fine and to push on with the appointment. But instead, we sat and explored his concerns. We asked each other questions and we sat through conversation and silences that were uncomfortable for the both of us. We came to an agreement that we would get his hearing aids as good as they can be for his dementia assessment, so that we can face things confidently with our heads held high.

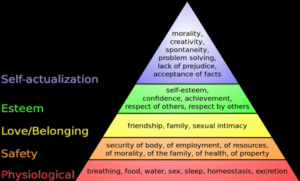 YES: Review Maslow’s Hierarchy of Needs
YES: Review Maslow’s Hierarchy of Needs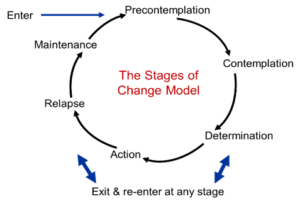
 Paul Peryman, MA, Dipl Aud (Melb), MNZAS-CCC, Audiologist
Paul Peryman, MA, Dipl Aud (Melb), MNZAS-CCC, Audiologist



 Diana Harbor, BA
Diana Harbor, BA Yesterday I had the privilege of being with a group of teenagers all living with hearing loss, using different technology from cochlear implants to bone implanted devices with different personalities and experiences of the world, some who had never met each other before. We all took part in an exciting improv, drama workshop at the Ear Foundation. Much of the afternoon was spent in small groups creating wonderful stories and weaving a single idea into a feast of creativity that JK Rowlings would have drooled at. And the real magic happened as Loydie, a DJ from Capital radio, revealed to us very simple techniques for keeping ideas going, for turning problems into new ideas and for getting the best out of each other. The power of using the phrase “…yes and” and how to do this while listening and maintaining eye contact.
Yesterday I had the privilege of being with a group of teenagers all living with hearing loss, using different technology from cochlear implants to bone implanted devices with different personalities and experiences of the world, some who had never met each other before. We all took part in an exciting improv, drama workshop at the Ear Foundation. Much of the afternoon was spent in small groups creating wonderful stories and weaving a single idea into a feast of creativity that JK Rowlings would have drooled at. And the real magic happened as Loydie, a DJ from Capital radio, revealed to us very simple techniques for keeping ideas going, for turning problems into new ideas and for getting the best out of each other. The power of using the phrase “…yes and” and how to do this while listening and maintaining eye contact.

 Jeanine Doherty, Au.D., M.Phil., M.B.S, B.Soc.Sci.(Hons.),
Jeanine Doherty, Au.D., M.Phil., M.B.S, B.Soc.Sci.(Hons.),  As we know, ethics, legality and morality are each different, though related, constructs. Something can be legal, yet immoral to an individual, as our values lead to our personal morals. Moral distress arises when clinicians are unable to act according to their moral judgement and their Profession’s Ethical Code (Rodney, 2017). This distress is located not only within individuals when their actions mismatch their values, but also from within the broader healthcare structures of the clinician’s workplace. The socio-political structures that can create moral/ethical distress have been studied mostly within nursing, but the relevance of the concept to audiology should not be ignored. Moral distress also emerges from situations that are against all the principles of PCC.
As we know, ethics, legality and morality are each different, though related, constructs. Something can be legal, yet immoral to an individual, as our values lead to our personal morals. Moral distress arises when clinicians are unable to act according to their moral judgement and their Profession’s Ethical Code (Rodney, 2017). This distress is located not only within individuals when their actions mismatch their values, but also from within the broader healthcare structures of the clinician’s workplace. The socio-political structures that can create moral/ethical distress have been studied mostly within nursing, but the relevance of the concept to audiology should not be ignored. Moral distress also emerges from situations that are against all the principles of PCC.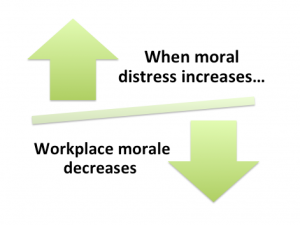 Harris and Griffin (2015) write that some organisational policies can lead to diminished care quality and cynicism with lack of teamwork and lower morale amongst clinical staff. In such a work-place, increased competition and mistrust develops between staff, while middle management level finds itself stuck between demands from higher-up levels (e.g. profit/cost outcomes) and the lack of teamwork and lower morale of the clinicians who are in moral distress. The physiological and psychological effects caused by the existence of moral distress can lead to burn-out, and then the staff member becomes ill, finds another better workplace, or just gives in, morally disengages, and carries on in a manner that is opposed to their values/morals (Musto, Rodney & Vanderheide, 2015). Lachman’s (2016) list of symptoms of burnout includes fatigue, general illness, headaches, insomnia, disillusionment, anger, negative self-concept and a loss of concern for others.
Harris and Griffin (2015) write that some organisational policies can lead to diminished care quality and cynicism with lack of teamwork and lower morale amongst clinical staff. In such a work-place, increased competition and mistrust develops between staff, while middle management level finds itself stuck between demands from higher-up levels (e.g. profit/cost outcomes) and the lack of teamwork and lower morale of the clinicians who are in moral distress. The physiological and psychological effects caused by the existence of moral distress can lead to burn-out, and then the staff member becomes ill, finds another better workplace, or just gives in, morally disengages, and carries on in a manner that is opposed to their values/morals (Musto, Rodney & Vanderheide, 2015). Lachman’s (2016) list of symptoms of burnout includes fatigue, general illness, headaches, insomnia, disillusionment, anger, negative self-concept and a loss of concern for others. Laya Poost-Foroosh, PhD., MClSc.
Laya Poost-Foroosh, PhD., MClSc.



 Georgina Aidoo
Georgina Aidoo usually does not command much attention in third world countries, even though various studies and estimates indicate that two-thirds of the world’s populations of hearing impaired people live in the developing countries. In many African countries, the general awareness of Audiology and hearing loss management is low, and lack of resources, ignorance, illiteracy, cultural diversity and national priorities among many other factors relating to technology enhancement and sense of focus has caused a lack of strong advocacy in this area. The Africa continent has a predominantly young population and many are at risk of getting diseases causing hearing loss (McPherson & Holboro, 1985). Overall, it is estimated that in the countries below Sahara, more than 1.2 million children aged between 5 and 14 years suffer from moderate to severe hearing loss in both ears. General prevalence studies show higher rates of severe to profound hearing loss in this part of Africa than in other developing countries.
usually does not command much attention in third world countries, even though various studies and estimates indicate that two-thirds of the world’s populations of hearing impaired people live in the developing countries. In many African countries, the general awareness of Audiology and hearing loss management is low, and lack of resources, ignorance, illiteracy, cultural diversity and national priorities among many other factors relating to technology enhancement and sense of focus has caused a lack of strong advocacy in this area. The Africa continent has a predominantly young population and many are at risk of getting diseases causing hearing loss (McPherson & Holboro, 1985). Overall, it is estimated that in the countries below Sahara, more than 1.2 million children aged between 5 and 14 years suffer from moderate to severe hearing loss in both ears. General prevalence studies show higher rates of severe to profound hearing loss in this part of Africa than in other developing countries. The case of Ghana is no different. In spite of the fact that hearing and balancing disorders are common among persons in communities in Ghana, very few studies have been carried out. The pace of development is very slow despite how critical the need is.
The case of Ghana is no different. In spite of the fact that hearing and balancing disorders are common among persons in communities in Ghana, very few studies have been carried out. The pace of development is very slow despite how critical the need is.