 Kris English, PhD
Kris English, PhD
The University of Akron/NOAC
Audiologic counseling is like a two-sided coin: one side attends to patients’ emotional and psychological struggles, and the other side, to their need for clear, relevant, and compelling information. Goleman (1995) would describe these two goals as communicating either with the “feeling mind” or the “thinking mind.” The concept of “being of two minds” is a familiar one, but communicating with a patient’s “thinking mind” (more specifically, our efforts in patient education) hasn’t attracted much attention in audiology.
Patient education can be taken for granted, but that would be a grave mistake. If not careful, we might apply a range of ineffective practices, such as:
- Using words our patients can’t process;
- Providing more detail than patients can remember;
- Conveying information unrelated to patients’ questions;
- Providing information without helping patients apply it to their lives.
Let’s ponder that last point for a moment. Information designed to “help patients apply it to their lives” elevates patient education to a new level of responsibility. We are not only talking about providing information, but also using information as a vehicle for change.
This concept is relatively new. Falvo (2011) notes that while “many people think of patient education as the transfer of information … the real goal is patient learning, in which patients are not only provided with information, but helped to incorporate it into their daily lives” (p. 21). We are being invited to redefine this process, to evolve from a monologue of information-giving into an interactive framework for change.
The concept of “effective patient education” can be new territory for many audiologists. How do we find our way? This article outlines a suggested checklist to guide us, applying classic teaching/learning principles culled from exemplar patient education materials.
A Checklist for Audiology
Patient education has a familiar starting point: knowledge dissemination.
Knowledge Dissemination. We have much information to share about test results, anatomy, etiologies, genetics, recommendations, treatments. However, as part of effective patient education, this step is just the first of several considerations. Even as we disseminate information, we cannot assume the patient understands us, or will remember what we said accurately. Let’s consult this checklist of concerns:
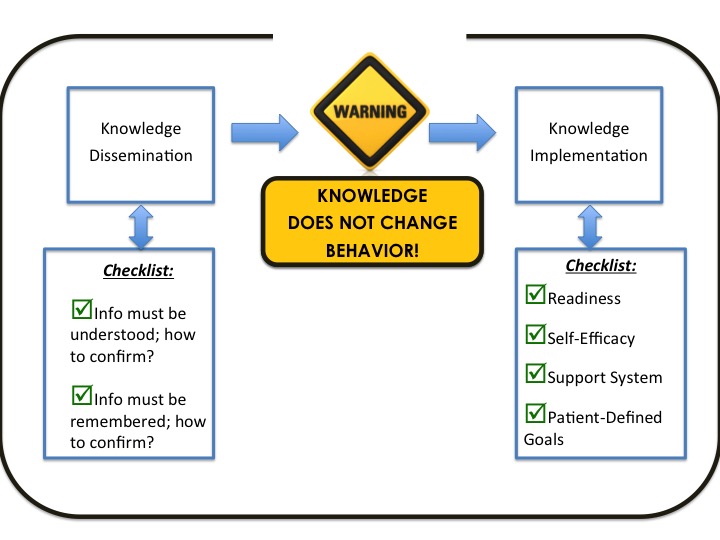
As we disseminate knowledge:
Does our patient understand us? In addition to the problems with professional jargon, we must remember that when a patient is upset, the amgydala in the brain activates “flight or fight” responses (increased heart and respiration rates, etc.). While in this state, the frontal cortex (the center for analysis and reasoning) is inaccessible. We might be talking to a brain that, for the time being, cannot learn. How to test for understanding? The easiest way is to ask: “Would you like a detailed explanation, or a big-picture summary? Do you prefer information conveyed verbally, or in writing, or both?” And later, “To be sure we are on the same page: could you share with me your understanding of the situation?” Asking the patient to repeat what they understand is called the “teach-back method” (Agency for Healthcare Research and Quality, 2010).
Will our patient remember what we said? Working memories are limited even in our best moments. Converting short memory traces to long-term memory depends on repetition and review; otherwise, the neural cells that had been temporarily excited will reset itself and act as if nothing happened (Medina, 2008). Solutions include easy-to-read handouts to take home for later review; lists of websites with relevant video demonstrations or patient/parent testimonials; intentional review of the information in follow-up appointments.
After Knowledge Dissemination: Warning! Even after confirming our patients understand us and can recall details later, there is no reason to expect them to act upon the information we have shared. As the warning sign in the middle of the checklist reminds us: “Knowledge does not change behavior.” We see examples of this tendency everyday: people smoke even though fully aware of the health risks; drivers text even after hearing of yet another fatal accident. Patients hesitate to improve their hearing status even as they acknowledge their social isolation. Change means making choices, but when given choices, humans tend to choose inertia (Thaler & Sunstein, 2009). Knowing that “no action” is a likely response, we actively add another step to patient education: knowledge implementation. This step takes the patient’s perspective as a learner into account.
Knowledge Implementation. This second step in effective patient education aims to “help patients help themselves.” The following checklist items are inter-related; each item is designed to engage the patient as a partner in the change process.
Readiness. No one does anything until they are ready. A simple way to discuss this variable is the classic 1-10 scale. If 1 means “no way” and 10 means “ready right now,” what will a patient say when we ask, “How ready are you to try hearing aids, use communication repair strategies, advocate for yourself?” Patients are more likely to give high numbers when they perceive themselves in a safe environment and have a social support system (mentioned below). If they give low numbers, we can ask, “What keeps you at a 2? What would move you up to a 5 or 6?” We won’t know until we ask – and the patient may not know until he or she begins to explain. These conversations help create that safe environment mentioned above.
Self-efficacy. When confronted with change, patients will ask themselves a very reasonable question: “Can I do this?” That is, do I believe in my ability to control my desired outcomes? Self-efficacy does not depend on “being smart,” but on knowing one can control one’s effort and persistence (Elliot & Dweck, 2007). To help patients answer the question, we can ask them for examples in their past when they successfully dealt with similar challenges. “Small wins” provide concrete evidence that a task is within one’s abilities. Our patient education plan can sketch out manageable steps (using hearing aids in a quiet restaurant, then in a movie, etc.), and help patients recognize measurable improvement.
Support System. The value of social support cannot be underestimated (Taylor, 2002). However the patient defines it, find a way to incorporate valued people into the learning process.
Patient-Defined Goals. When we confirm that the patient is ready to use our information, believes in his or ability to do so, and has a support system to help with the process, we are ready to focus on goals. Effective patient education requires the patient, not the audiologist, to identify the problems to solve and the goals to accomplish. These goals represent the patient’s internal motivation and personal expertise. When the goals are identified, the audiologist’s role is to teach appropriate problem-solving skills and help the patient test them out.
Conclusion
We audiologists describe ourselves as clinicians, scientists, problem-solvers, helpers – and, although often unacknowledged, we are also educators. Since the educational component represents a significant part of our practices, we are of course obligated to educate effectively. Today’s health care environment defines effective patient education to include both the dissemination and implementation of knowledge – the latter involving an understanding of change. This proposed checklist is offered as a springboard for future discussion, as we continue to explore our role in audiologic counseling.
Author note: The above is adapted from: © English, K. (2011). Effective patient education: A roadmap for audiologists. ENT & Audiology News, 20(4), 99-100.
References
Elliot, A.J, & C.S. Dweck, C.S. (Eds.). Handbook of competence and motivation. NY: Guildford Press.
Falvo, D. (2011). Effective patient education: A guide to increased adherence (4th ed.). Sudbury, MA: Jones & Bartlett.
Goleman, D. (1995) Emotional intelligence: Why it might matter more than IQ. New York: Bantam Books.
Medina, J. (2008). Brain rules. Seattle: Pear Press.
Taylor, S. (2002). The tending instinct: How nurturing is essential to who we are and how we live. New York, NY: Henry Holt.
Thaler, R.T., & Sunstein, C.R. (2009). Nudge: Improving decisions about health, wealth, and happiness. New York: Penguin Books.
This entry was posted in Faculty by admin. Bookmark the permalink.
