 Kris English, PhD
Kris English, PhD
The University of Akron/NOAC
As mentioned in Part 1/5 and Part 2/5 of this series, Stewart et al. (2014) provide a framework to implement Patient Centered Care (PCC), organized around four interactive components. In this entry, we will consider the 2nd component, Understanding the Whole Person.
Understanding: Patient-as-Person
Already we are seeing the interactive nature of each component, since the first PCC component encourages us to “explore” by finding out about our patients. Relative to their hearing circumstances, what are their personal backgrounds, their current situations, and what is important at this time? A person’s life- and world-context matters for everybody, but particularly for our patients, whose hearing loss can have direct impact on their life and their world. Factoring those contexts into our understanding of the “whole person” is considered “a hallmark of the patient-centered clinician” (Stewart et al., p. 89)
Understanding: Patient-in-Context
The additional layer to this component is understanding the patient as part of an eco-system, in a way. “Proximal context” generally includes one’s immediate family and other important persons in our patient’s living circumstances. Expanding outward, we would like to know about living circumstances (neighbors, care-givers), employment status and associated listening challenges; social supports within one’s community, and so on. Additionally, “distal context” may be relevant to many patients, if their culture and community play an active part in their life.
 “Listen and Learn” — But Don’t Stop!
“Listen and Learn” — But Don’t Stop!
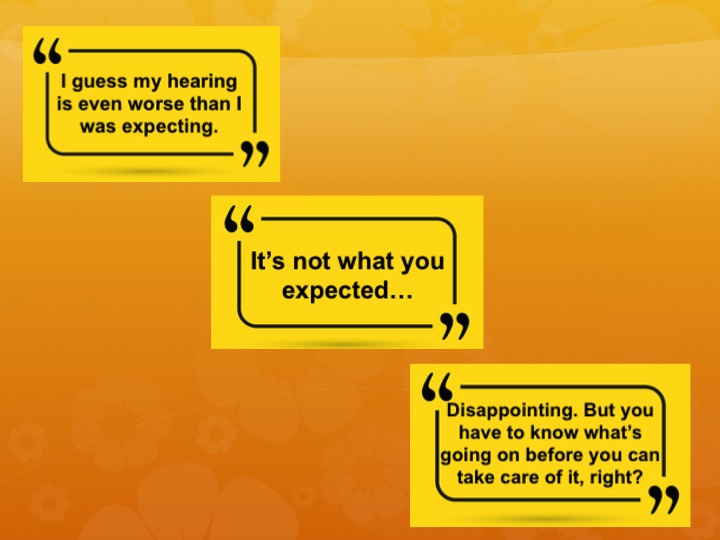
There is more to the “understanding” component than meets the eye. To be of any value, our understanding must be actively communicated to the speaker. Merely listening and processing the input does not help a patient “feel heard.” We must actively respond. Consider these details from a study that tracked patient comments, subsequent physicians’ responses, and ultimate patient outcomes to get a sense of how important it is to actively convey understanding.
Adams et al. (2012) recorded, transcribed, and evaluated 79 patient-physician office visits. They identified 190 instances of patients expressions of emotional state, coded the physicians’ responses, and then categorized the responses as follows:
- Responses that focused away from emotion
- Neutral (Focused neither away from or toward)
- Responses that focused toward emotion
They also took the additional step of evaluating consequences: what were the outcomes relative to patient care? The flow chart below tracks the three “response choices.” When physicians ignored patient emotions, outcomes were unproductive at best: when distance and even antagonism develops, we know we are going in the wrong direction. However, when physicians responded to emotions (i.e., what patients actually wanted to talk about) with neutral or actively focused responses, outcomes were productive: additional discussion led to a confirmation of goals; support was conveyed; patients and physicians understood they were on the same page.
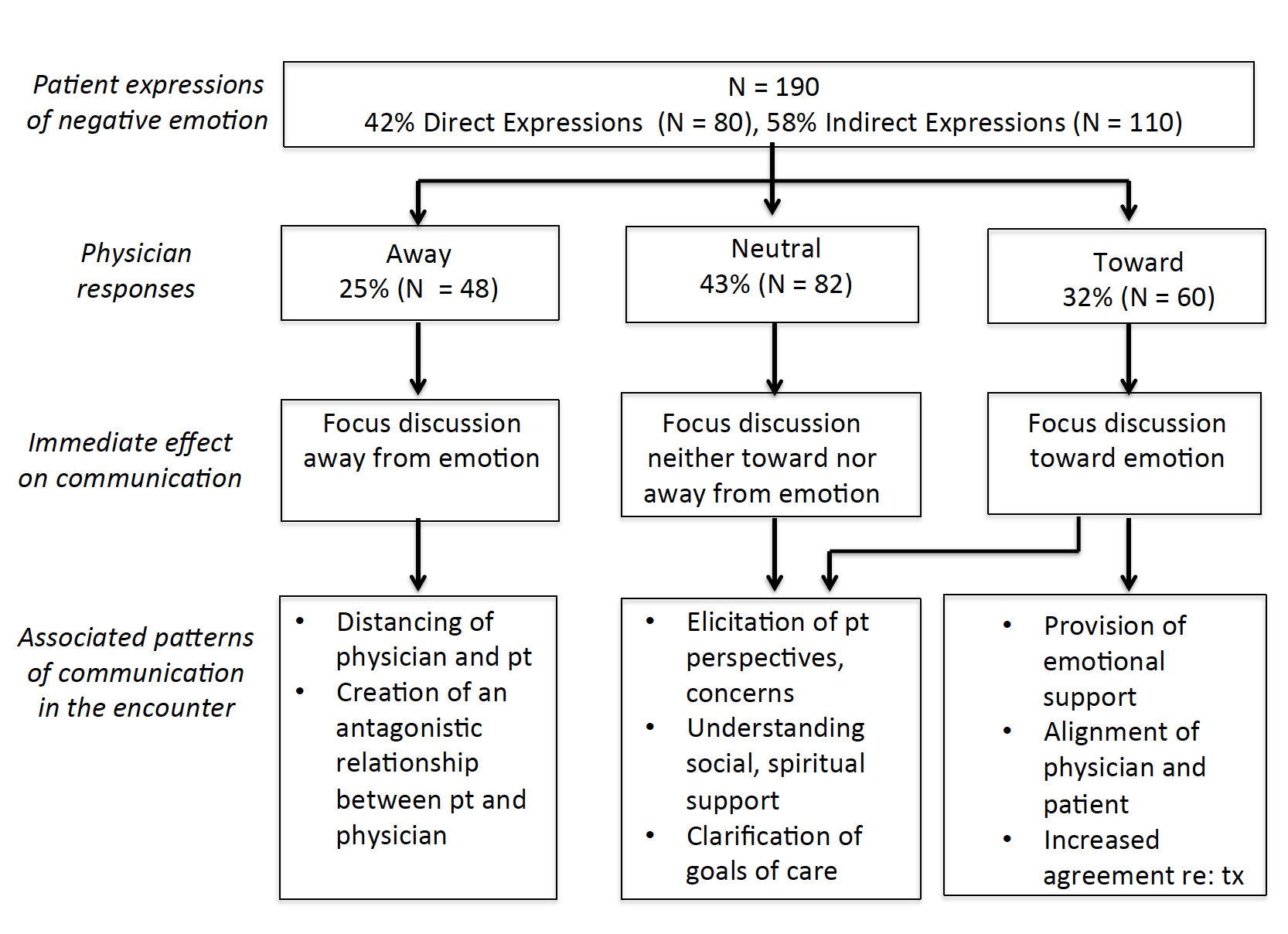
Fig. 1. Physician responses to patients’ expressions of emotion: immediate effect on communication and associated patterns of further communication. (Adams et al,, 2012, p. 47)
Did Responses Make a Difference?
Of course they did. Let’s assume that physicians in the first column of boxes did hear their patients’ emotional concerns, but simply failed to respond in an active way to let the patients (and the researchers) perceive it. It is quite easy to become distracted, anticipate other topics, notice the time and rush ahead. But missed opportunities have consequences; our efforts to be patient-centered must keep “active understanding” a high priority.
Following are three tips to support our endeavors to convey understanding:
Active Understanding Tip #1: Use Observable (Measurable) “Understanding Responses” 
The following kinds of responses are within everyone’s repertoire; the only concern is remembering to communicate them. Recommendations from the Patient-Centered Observation Form (PCOF) (Keen et al. 2015) include:
- Use continuer phrases (OK; hmm-mm) and attentive body language
- Validate emotions (you’re worried about changes; it sounds like you were uncomfortable?)
- Elicit more input (Could you help me understand with an example? Anything else?)
- Confirm what is most important to patient (So let me confirm: you indicated the following problems need our attention…)
Audiologists interested in improving this skill might consider partnering with a colleague to observe/count instances of active understanding by using the PCOF.
Active Understanding Tip #2: Include Family
Research (e.g., Singh et al. 2016) consistently supports the value of including family members (“proximal context”) in audiology appointments. This essay provides some food for thought.
Active Understanding Tip #3: Try Ida Institute’s Communication Rings
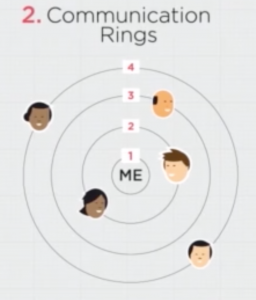
This easy-to-easy and literally patient-centered tool helps the audiologist understand not only our patients’ family/”proximal” contexts but also their “distal” contexts. Organizing and prioritizing one’s “communication world” has the double benefit of helping both the audiologist and the patient understand the impact of hearing loss.
PCC is a Process
At this point, we see that Patient-Centered Care does not involve a singular change in practice, but rather a commitment to an integrated process. We have applied the first two steps to audiology; the next steps will be examined in Parts 4/5 and 5/5
The Ultimate Question: Is “Active Understanding” an Evidence-Based Practice?
See Tzelepis et al. (2015) to learn more.
NEXT: Audiology Counseling and Patient-Centered Care, Part 4/5: Common Ground

- I routinely inquire about a patient’s proximal and distal contexts.
Almost always Sometimes I tend to skip this step
- I am aware of the risks of not actively conveying understanding about a patient’s emotional responses to hearing loss.
Fully aware Sometimes aware Hadn’t realized it until now
- I would find it helpful to review my responses to determine if they conveyed active understanding.
Yes Not sure
- I actively include family members in appointments (per patient preference).
Almost always Sometimes I often skip this step
- I can explain why “active understanding” is an evidence-based practice.
Yes Still working on it
References
Stewart, M., Brown, J.B., Weston, W.W., McWhinney, I.R., McWilliams, C.L., & Freeman, T.R. (2014). Patient centered medicine: Transforming the clinical method (3rd ed.). London: Radcliff Publishing.
