 Kris English, PhD
Kris English, PhD
Professor Emeritus
The University of Akron
We all know that childhood bullying is nothing new. However, we now also know a great deal about the long-lasting effects of bullying victimization. Longitudinal cohort studies indicate that children with a history of being bullied are at increased risk for overall mental and physical health problems, anxiety, depression, and self-harm — toxic stress responses that extend far into adulthood (Copeland et al., 2013; Lereya et al., 2015).
The U.S. Department of Education (2011) has identified bullying as a public health/public safety issue, and Takizawa et al. (2014) have framed it in the clearest possible language: “Victimization by bullies is increasingly considered alongside maltreatment and neglect as a form of childhood abuse” (p. 777). Excuses such as “kids will be kids” and “bullying is just a rite of passage” can no longer be tolerated.

As part of a child’s support system, we must understand that children who are being bullied might hesitate to ask for help, for a variety of reasons: embarrassment, fear of retribution, or worry that adults will make the situation worse. They may not even be sure of the difference between “tattling” (which they’ve been taught they should not do) and telling an adult about being bullied. Bauman and Pero (2010) unsurprisingly found that children with hearing loss were just as likely as other children to “not tell.”
Rather than wait for a child to disclose a problem, the American Academy of Pediatrics (AAP) (2009, 2017) adopted a policy to routinely screen for bullying concerns as a standard of care. Squires and colleagues (2013) have advocated for audiologists to assume the same responsibility. But how to broach this sensitive subject?
First, Do Our Homework
We should not screen for bullying until we have some basic information:
⇒ Review StopBullying.Gov for important information on “red flags,” at-risk children, cyberbullying, a child’s legal rights to a safe environment at school (Norlin, 2015), and bullying concerns outside of school.
⇒ Learn local laws and policies re: anti-bullying programs in the child’s school, and communicate with school administration when possible.
⇒ Develop a support team at your setting, and ensure you are ready for “next steps” should a child disclose a concern, including self-harm. We should not screen until we are comfortable with the unpredictable nature of the subsequent conversation.
A Screening Conversation
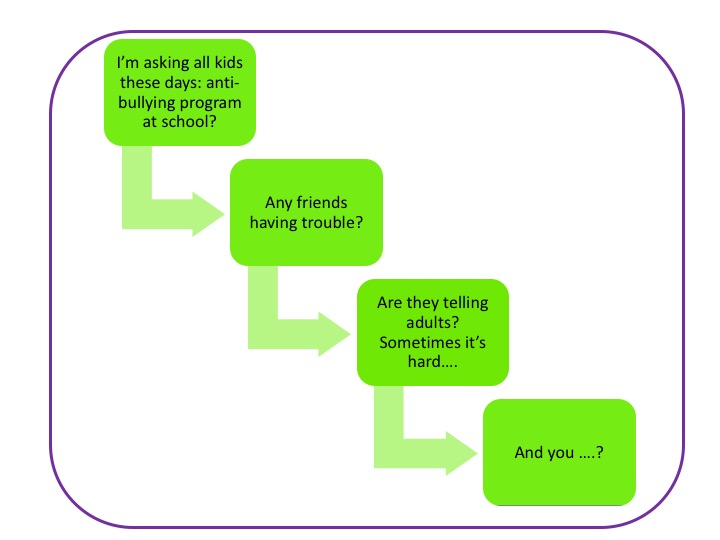
The following bullets and flowchart can be used to frame the screening conversation (Clark & English, 2019). The approach starts from a safe and general context, shifting to a child’s social circle, and eventually to the child him/herself:
- Here in our clinic, we now have a question we ask every child these days, and I hope you will help me with it. I understand all schools have a bullying prevention program; can you tell me about yours?
- (If little information is shared, some follow-up questions include: is there a safety officer? Posters around school about being safe? What do you think about the program?)
- (If the audiologist is working in a school, the opening question would address the on-site program: We have a program here, but we always want to check to see what children think about it. Do you think it works, etc?)
- Do any of your friends have problems with a bully?
- If it happens, do your friends know what to do/who to talk to?
- How about you: do you know any bullies? Do they bother you…?
 As We Screen:
As We Screen:
Children may hesitate to describe a situation as bullying. We are listening for:
- An imbalance of power
- Ongoing recurrences
- Intentional rather than accidental behavior
- Behaviors that cause mental, social, emotional, or physical harm
- Any sign of distress
Our follow-up steps:
- Let the child know we will help
- Communicate concerns with parent/caregiver (who may need help bringing the concern to school officials)
- Share information on strengthening the child’s IEP (see Hands&Voices.org)
- Monitor the child’s well being and school responses
- Keep referral systems up-to-date: a child could be in a crisis situation and considering harm to self or others.
- Document
- Note: If working in a medical setting, the AAP recommends adding a screening query to the electronic medical records system, not only to document but also establish the process as a standard of care.
A Matter of Urgency

If the reader has any concerns or questions about this topic, please do not hesitate to contact the author.
7.5 Tier 1 CEUs in Counseling Available Here!
References
American Academy of Pediatrics. (2017). Protecting youth from bullying: The role of the pediatrician.

