Kris English, PhD
Professor Emeritus, Audiology
The University of Akron
Should we complete a self-assessment on implicit bias such as the Implicit Association Test (IAT)? It’s a complicated question: the reliability and validity of the IAT has been established1,2 even as criticisms persist.3,4 And the uncomfortable prospective of finding out about our biases can keep us from considering the issue altogether….
Practically speaking, it may help us move forward by directly working with these “Key Characteristics of Implicit Bias” from the Kirwin Institute for the Study of Race and Ethnicity:
- Implicit biases are pervasive. Everyone possesses them, even people with avowed commitments to impartiality such as judges [and health care providers.]5
- The implicit [unconscious] associations we hold do not necessarily align with our declared beliefs or even reflect stances we would explicitly endorse.6
- Implicit biases are malleable. Our incredibly complex brains not only formed implicit associations during our childhood years, but can also gradually unlearn those biases through a variety of debiasing techniques.7
The last point is our focus here: that is, techniques to help us unlearn implicit biases. The following debiasing practices are adapted from Blair et al.8 and Cox & Devine9 as a self-managed, evidence-based, habit-breaking intervention. Each step is intended to slow down our thinking, keep us in the moment, and increase our ability to override our unconscious reactions.
First, some “brain warm-ups,” also known as cognitive priming:
“Cognitive Priming”
- Acknowledge that no one is bias-free.
- Learn how implicit biases can impact health care outcomes (see “Resources” below).
- Address rather than suppress uncomfortable feelings and thoughts associated with these insights.
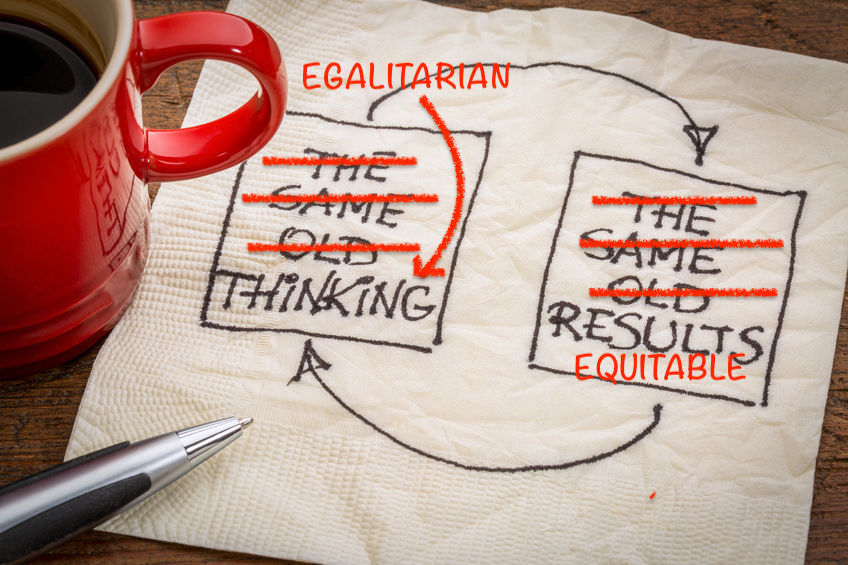
- Consciously affirm personal egalitarian goals.
- Rationale: Affirming our goals and values eases our defensiveness and promotes patient trust10
- Example of egalitarian goals: “People should be treated as equals, should treat one another as equals, should relate as equals, and enjoy an equality of social status”11
Mindful Efforts During Clinical Encounters
- Think Before Acting:
- Individuation: Imagine what it would feel like to be in the position of a member of a different group. Actively see the person as an individual rather than a stereotype.12
- Perspective taking, i.e., “putting yourself in the other person’s shoes13
- Even better: perspective-getting
- During Clinical Encounters:
- As we listen: rather than jumping to stereotypical assumptions, ask ourselves what other possibilities might account for behavior? Keep in mind the complexity of people’s lives.
- As we build partnerships: if we are not doing so, strive to reframe the interaction as a collaboration between equals, rather than between a high-status person and a low-status person (recall egalitarian goals).
- Post-Encounter Reflection:
- Journaling, or discussion with like-minded peers or other positive peer support system.14
- New habits require continuous practice, feedback, and reflection before they become second nature.15, 16
Conclusion: Implicit Bias ≠ Destiny
Take-away #1: Implicit bias is a mental habit, and habits can be changed.
Take-away #2: Changing habits is not easy, but our egalitarian goals (treating all persons as equals) can serve as “the better angels of our nature” (U.S. President Abraham Lincoln’s 1861 Inaugural Address).
Take-away #3: Readers will immediately recognize that each strategy described above is fully consistent with patient-centered communication and audiologic counseling. The goal remains the same: to communicate our commitment to making a personal connection, earning trust, and developing a partnership.
Resources
Kirwan Institute for the Study of Race and Ethnicity, The Ohio State University

How to Outsmart Your Own Unconscious Bias
The Problem with Race-Based Medicine
White, A., (2019). Seeing patients: A surgeon’s story of race and medical bias (2nd ed.). Cambridge, MA: Harvard University Press.
For More on Cultural Humility:
Part 4: Perspective-Getting/Radical Empathy
References
- Greenwald, A.G., et al. (1998). Measuring individual differences in implicit cognition: the implicit association test. Journal of Personality and Social Psychology, 74(6), 1464–80.
- Greenwald, A.G., et al. (2009). Understanding and using the Implicit Association Test: III. Meta-analysis of predictive validity. Journal of Personality and Social Psychology, 97(1), 17–41.
- Arkes, H. & Tetlock, P. (2004). Attributions of implicit prejudice, or “Would Jesse Jackson ‘Fail’ the Implicit Association Test?” Psychological Inquiry, 15(4), 257 278. DOI: 1207/s15327965pli1504_01
- Meissner F., & Rothermund K. (2015). A thousand words are worth more than a picture? The effects of stimulus modality on the Implicit Association Test. Social Psychological and Personality Science, 6(7), 740-748. doi:1177/1948550615580381
- FitzGerald, C., & Hurst, S. (2017). Implicit bias in healthcare professionals: A systematic review. BMC Medical Ethics, 18(19). DOI 10.1186/s12910-017-0179-8
- Chapman, E., et al. (2013). Physicians and implicit Bias: How doctors may unwittingly perpetuate health care disparities. Journal of General Internal Medicine, 28(11), 1504–10. DOI: 10.1007/s11606-013-2441-1
- Devine, P., et al. (2012). Long-term reduction in implicit race bias: A prejudice habit-breaking intervention. Journal of Experimental Social Psychology, 48, 1267-1278.
- Blair, I., et al. (2011). Unconscious (implicit) bias and health disparities: Where do we go from here? The Permanente Journal, 15(2), 71-78.
- Cox, W., & Devine, P. (2019). The prejudice habit-breaking intervention: An empowerment-based confrontation approach. In R. Mallett & M.J. Monteith (Eds.), Confronting prejudice and discrimination: The science of changing minds and behaviors(pp. 249-274). London, UK: Academic Press.
- Moskowitz, G & Li, P. (2011). Egalitarian goals trigger stereotype inhibition: A proactive form of stereotype control. Journal of Experimental Social Psychology, 47, 103-116.
- Stanford Encyclopedia of Philosophy. (n.d.).
- Burgess, D., et al. (2007). Reducing racial bias among health care providers: Lessons from social-cognitive psychology. Journal of General Internal Medicine, 22, 282-287.
- Todd, A.R., & Galinsky, A.D. (2014): Perspective-taking as a strategy for improving intergroup relations: Evidence, mechanisms, and qualifications. Social and Personality Psychology Compass, 8, 374–387. DOI: 10.1111/spc3.12116
- Sukhera, J., et al. (2018). Adaptive reinventing: implicit bias and the co‑construction of social change. Advances in Health Science Education, 23, 587-599.doi: 10.1007/s10459-018-9816-3
- Byrne, A., & Tanesini, A. (2015). Instilling new habits: Addressing implicit bias in healthcare professionals. Advances in Health Science Education, 20,1255-1262. DOI 10.1007/s10459-015-9600-6
- Monteith,M.J., et al. (2009). Schooling the cognitive monster: The role of motivation in the regulation and control of prejudice. Social and Personality Psychology Compass, 3, 211–226.
