 Kris English, PhD
Kris English, PhD
Professor Emeritus, Audiology
The University of Akron
Supervising audiology students is always rewarding. When it comes to supporting a student’s development in counseling skills, it is also complicated. “Teachable moments” often depend on personally observing a missed counseling opportunity, immediately modeling a relevant person-centered response, and then carving out time to discuss it later – but it is unknown if the student is better prepared for the next time (Fanai et al, 2018). Feedback provided at the end of the day (e.g., with the “Four Habits Rubric” [Saltrøe et al, 2021]) is helpful but still leaves professional growth more to chance than to pedagogical planning. Either way, the process places the student in a passive role.
Positioning the Learner to Take the Lead
In classroom instruction, students are provided syllabi that explicitly describe what they need to do to master course content, giving them agency over their outcomes. How to provide students agency re: counseling skill development in clinic? To address the limitations described above, healthcare educators are applying Bandera’s (1977) concept of self-efficacy. He defined self-efficacy as “people’s judgments of their capabilities to organize and execute courses of action required to attain designated types of performances. It is concerned not with the skills one has but with judgments of what one can do with whatever skills one possesses” (1986, p. 391). More simply, “The factors that influence behavior are embedded in the belief that one has the capability to accomplish that behavior” (Klassen & Klassen, 2018, p. 76).
possesses” (1986, p. 391). More simply, “The factors that influence behavior are embedded in the belief that one has the capability to accomplish that behavior” (Klassen & Klassen, 2018, p. 76).
We rarely highlight “belief” in audiology, but we do refer to it indirectly when we ask students to reflect on past challenges, what they learned about themselves, and how they apply that learning when new challenges arise (what they believe they are capable of accomplishing)(Zimmerman et al., 2017).
A Recent Application
In 2021, Wolderslund et al reported on delivering a communication skills program for healthcare professionals. Instead of measuring conventional learning outcomes (e.g., “What is the definition of shared decision-making?”), they applied Bandura’s concept of self-efficacy and asked attendees pre- and post-training questions such as, “How certain are you that you can successfully make a plan based on shared decisions between you and the patient?” Their pre-post assessment was a 12-item self-efficacy tool (SE-12) (Ammentorp et al, 2007; Norgaard et al, 2012), represented below. The items include well-known person-centered practices and use the word can to explore one’s sense of capability to achieve them.
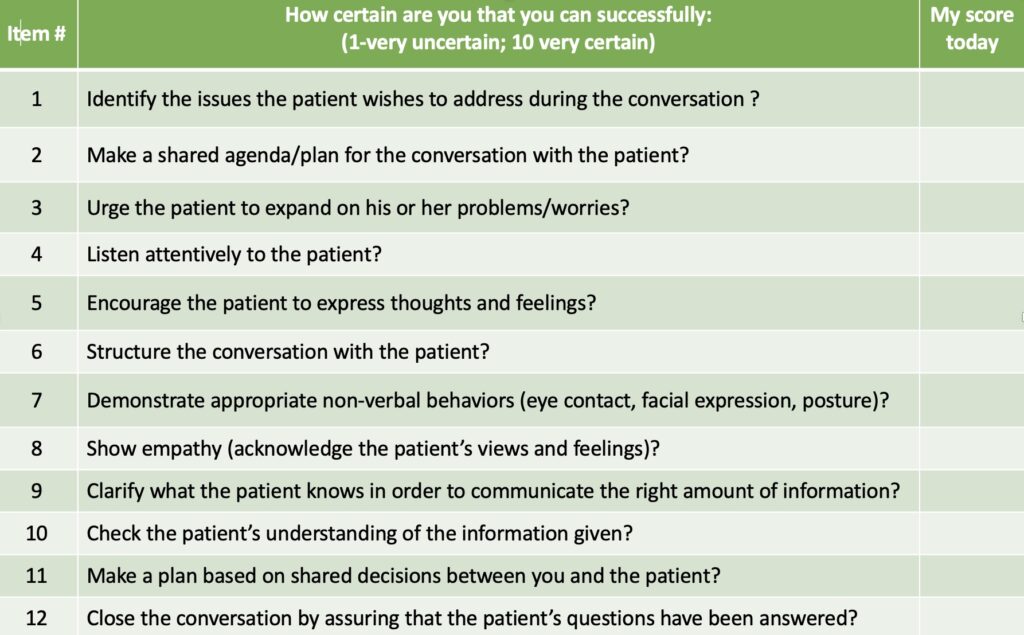
Self-Efficacy (SE) 12 (Wolderslund et al, 2021)
The SE-12 is a valid and reliable tool (Axboe et al, 2016), and is applicable to most healthcare training situations, including audiology. For example: students would complete a baseline SE-12 at the beginning of their clinical placement, and then identify personally relevant goals, design an improvement plan, and learn how to evaluate and trust their progress. By end of term, they would provide meaningful documentation for the supervisor’s final assessment, while confirming to themselves their capability to develop counseling skills.
A Secondary Benefit
When students become comfortable with increasing their own sense of self-efficacy in counseling, it can become easier to carry over the concept to patient care. After all, self-efficacy is one of the variables that affect life with hearing loss: i.e., the belief that one can or cannot face and deal with the challenge. We often broach this psychological aspect when discussing recommendations (first-time device use, modifying existing devices, using communication strategies) by asking, “Now that we’ve reviewed options and agreed on a plan moving forward…How confident do you feel about it?” (Cuevas et al, 2019). We may only then learn about harbored doubts, distress, and perceived barriers that our patient had not disclosed before.
Conclusion
There is more to counseling, of course. The SE-12 items provide a framework for person-centered care – the “what to do.” The art of “how to do” these steps advances the learner to essential interpersonal/counseling skills, for example:
- Responding to patient emotions
- Attention to nonverbal communication
- Conversations about stigma
- Cultural humility
…just to name a few (Ammentorp et al, 2022). Developing a strong track record in managing person-centered care will enhance self-efficacy in mastering the many counseling nuances.
References
Ammentorp J et al. (2022). Translating knowledge into practice for communication skills training for health care professionals. Patient Educ Couns, 105, 3334-3338.
Axboe, MK et al. (2016). Development and validation of a self-efficacy questionnaire (SE-12) measuring the clinical communication skills of healthcare professionals. BMC Medical Educ, 16, 272. https://doi.org/10.1186/s12909-016-0798-7
Bandura, A. (1986). Social foundation of thought and action: A social cognitive theory. Englewood Cliffs, NJ: Prentice Hall.
Fanai JK et al. (2018). Performance feedback to increase use of counseling skills. Seminars Hrg, 39(1), 44-51.
Norgaard B et al. (2012). Communication skills training increases self-efficacy of health care professionals. J Contin Educ Health Prof, 32(2), 90–97.
Wolderslund M et al. (2021). The effectiveness of a person-centred communication skills training programme for the health care professionals of a large hospital in Denmark. Patient Educ Counseling, 104, 1423-1430.
Zimmerman B et al. (2017). The role of self-efficacy and related beliefs in self-regulation of learning and performance. In A. Elliot, C. Dweck, and D. Yeager (Eds.), Handbook of competence and motivation (2nd ed.) (pp. 313-333). New York: Guildford Press.
