Kris English, PhD
The University of Akron/NOAC
In Part 1 of this series, we considered empathy as an act of “sharing space” with another’s experience and emotional state. In Part 2, we highlighted the importance of actively checking our impressions of another’s experience and state, to avoid the disconnect of “rejected empathy.”
Taking this learning process to its logical conclusion, as educators we are charged to evaluate the development of these interpersonal skills. However, to date very little has been written in audiology as to how to go about it. Fortunately, there are several valid and reliable assessment tools (Batt-Rawden et al., 2013), including the Four Habits Coding Scheme, described and referenced below. Before testing out the Four Habits, though, let’s consider one habit not included on this rubric, a habit that we may need to break: a tendency to try to “make things better” by saying “at least.”
“At least” … Creating Distance, Not Sharing Space
Such a seemingly innocuous phrase! And yet, consider the following comments and their impact on empathy:
- At least we can improve your hearing problems with modern technology.
- At least we identified your child’s hearing loss early.
- Lots of people have hearing loss far worse than you do (“at least” is not spoken but implied).
On the surface, our intention is commendable: to help a patient or parent feel better (Lundberg & Lundberg, 1997). However, ironically, to say or imply “at least” only makes the speaker feel better, and at the same time diminishes the patient’s experience. By offering impersonal reassurances, we inadvertently distance ourselves from our patient. We convey access to some special knowledge, that we know more about the situation than the person experiencing it. Such distance-creating signals are inconsistent with what Carl Rogers (1979) called “the subordination of self.” Discuss!
impersonal reassurances, we inadvertently distance ourselves from our patient. We convey access to some special knowledge, that we know more about the situation than the person experiencing it. Such distance-creating signals are inconsistent with what Carl Rogers (1979) called “the subordination of self.” Discuss!
Applications to Audiology
Learning Objective #1: Catch/break the habit of saying “at least.”
Learning activity: View this 3-minute animated segment of a popular TED talk:
Brené Brown on Empathy.

- Give three examples of how an audiologist might be inclined to “empathize” with an “at least” response.
- Name three emotional reactions a patient or parent might experience when presented with an “at least” response.
Learning Objective #2: Evaluate empathy skills with a valid, reliable rubric.
Learning Activity: Ask students to self-evaluate their present ability to communicate empathy using one section of the “4 Habits Coding Scheme” (Jensen et al., 2010; Krupat et al., 2006), summarized in the table below. Conduct your own evaluation of each student and then compare notes. What seems to be your next step to improve empathy skills?
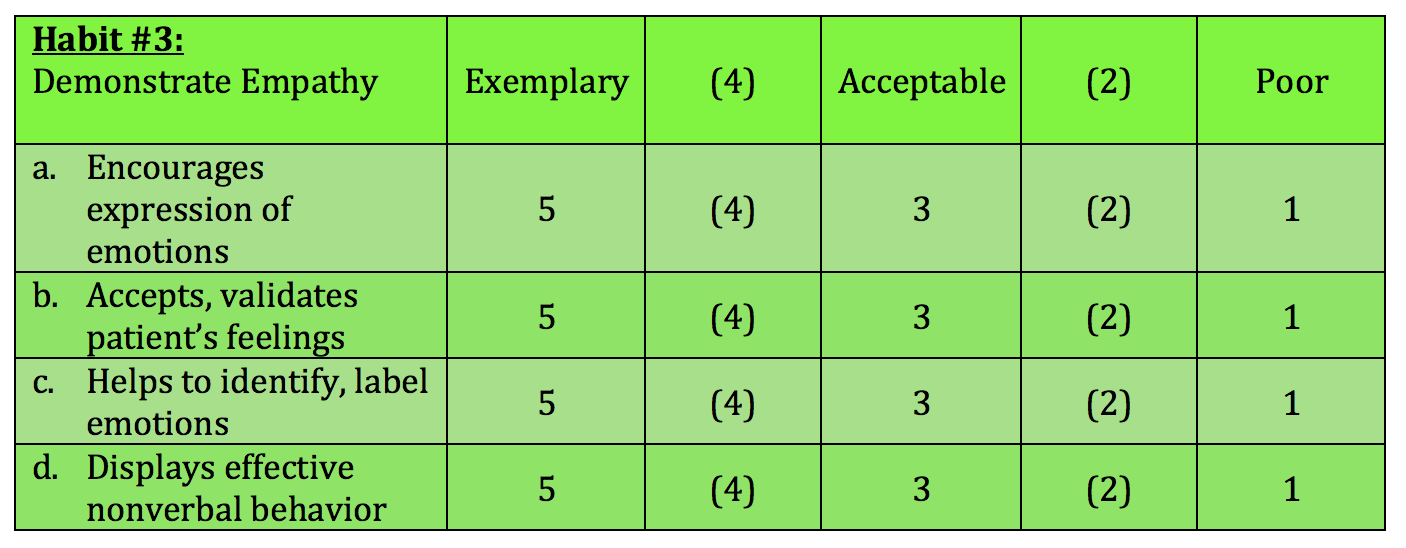
Coding Scheme: Code each item below using categories 1, 3 or 5. If you feel strongly that the behavior being coded is directly between these categories, use the values 2 or 4.
5 = Exemplary
- Clearly accepts/validates patient’s feelings (e.g., I’d feel the same way… I can see how that would worry you…)
- Makes clear attempt to explore patient’s feelings by labeling them (e.g., It seems to me you are feeling quite anxious about ….)
- Displays nonverbal behaviors that express great interest, concern, and connection (eye contact, tone of voice, body orientation) throughout appointment
3 = Acceptable
- Briefly acknowledges patient’s feelings but makes no effort to accept/validate.
- Makes brief references to patient’s feelings but does little to explore or label them.
- Nonverbal behaviors show neither great interest or disinterest (or behaviors over course of appointment are inconsistent)
1 = Poor
- Makes no attempt to respond to/validate the patient’s feelings, possibly belittling them (e.g., It’s ridiculous to be so concerned about …)
- Makes no attempt to identify patient’s feelings
- Nonverbal behavior displays lack of connection (e.g., little or no eye contact, body orientation or use of space inappropriate, bored voice)
(Sources:Jensen et al., 2010; Krupat et al.,2006; Lundeby et al., 2015)
A Final Thought (For Now)
When it comes to teaching empathy, Batt-Rawden et al. (2013) suggest we think about “walking the walk:”
Bayne (2011) highlighted the importance of role models and the reciprocal nature of empathy development in training, suggesting that “Indeed, perhaps students need to receive more empathy from faculty… before they can truly understand how to establish empathic connections.” Thus, educators should consider using the practice of relationship-centered care as the fundamental building block for their educational interventions to teach empathy” (p. 1175).
References
Bayne, H. (2011). Training medical students in empathic communication. The Journal for Specialists in Group Work, 36, 316-329.
Lundberg, G., & Lundberg, J. (1997). “I don’t have to make everything all better”: Six practical principles that empower others to solve their own problems while enriching your relationship. New York: Penguin Books.
Lundeby, T., Gulbrandsen, P., & Finset, A. (2015). The Expanded Four Habits Model – A teachable consultation model for encounters with patients in emotional distress. Patient Education and Counseling, 98, 598-603.
Rogers, C. (1979). Foundations of the person–centered approach. Education, 100(2), 98-107.
