 Kris English, PhD
Kris English, PhD
Professor Emeritus of Audiology
The University of Akron
On January 29, 2024, a Muppet character from the US television show “Sesame Street” posted a friendly query on social media: “Elmo is just checking in! How is everybody doing?”

https://sesameworkshop.org/our-work/shows/sesame-street/sesame-street-characters/elmo-2/
Initial responses were cheery and light-hearted, but soon more than 20,000 readers responded “from the heart,” describing loneliness, financial and health struggles, depression, and more. It was quickly observed that Elmo (via his handler) seemed to be channeling psychologist Carl Rogers by responding with empathy and warm acceptance (aka unconditional positive regard).1,2

President Joe Biden echoed Elmo’s empathy and warm acceptance: “I know how hard it is some days to sweep the clouds away and get to sunnier days. Our friend Elmo is right. We have to be there for each other, offer our help to a neighbor in need, and above all else, ask for help when we need it. Even though it’s hard, you’re never alone.” Links to several mental health services were also posted.
What About Congruence?
In addition to empathy and warm acceptance, students of Rogerian counseling theory will notice that a third “pillar,” congruence, was not mentioned in news reports – partly because it is “inward work,” not readily observable:3
- Persons who are congruent honestly understand their internal feelings and thoughts, which supports their ability to outwardly communicate empathy and warm acceptance to others.
- On the other hand, persons who are incongruent do not honestly understand their internal feelings and thoughts, which may include unaddressed biases of any kind.4
 Incongruence hinders our ability to communicate empathy and warm acceptance to persons associated with those biases, and efforts to do so come across as inauthentic.
Incongruence hinders our ability to communicate empathy and warm acceptance to persons associated with those biases, and efforts to do so come across as inauthentic.
When patients perceive inauthenticity, trust is difficult to establish – and as clinicians, we too are also aware when there is a disconnect, that at some level we “just don’t feel it for some reason.” The current call for increased awareness and management of implicit bias is consistent with the counseling principle of clinician congruence.5-7
Rogers’ Congruence Journey
 It would not be unusual for helping professionals to miss the impact of unconscious / implicit bias on congruence – even Carl Rogers seemed to have overlooked it until rather late in his career. Crisp8 recently reported on two video recordings of Rogers’ therapy sessions with two different Black male patients, conducted 5 years apart. The first session from 1979 was described by peers as having a “therapist-centric perspective” (p. 223) with missed opportunities to respond with empathy to the client’s racism experiences and avoiding an exploration about their racial and cultural differences.
It would not be unusual for helping professionals to miss the impact of unconscious / implicit bias on congruence – even Carl Rogers seemed to have overlooked it until rather late in his career. Crisp8 recently reported on two video recordings of Rogers’ therapy sessions with two different Black male patients, conducted 5 years apart. The first session from 1979 was described by peers as having a “therapist-centric perspective” (p. 223) with missed opportunities to respond with empathy to the client’s racism experiences and avoiding an exploration about their racial and cultural differences.
Subsequent experiences in cross-cultural workshops increased Rogers’ awareness of race-related issues and, as part of his commitment to ongoing examination of his unconscious assumptions, modified his definition of congruence to include an awareness of cultural diversity.9
His “reset journey” is perceptible in a second session recorded in 1984: “Rogers was confronted with a client whose difficulties with racism included Rogers himself being a white therapist… He communicated appreciation and respect for the client’s courage in speaking to him honestly, and for his rebellion against the racism in white America” (p. 230 ).
Conclusion
Congruence is obviously easy for Elmo, since he clearly doesn’t have a biased bone (or any bones!) in his body. For the rest of us, it’s an ongoing project… just as with Carl Rogers.
“Personal development in terms of congruence is considered to be a lifetime process needing devoted commitment and active effort” (p. 236).10

Salk Institute, La Jolla, California
References
- Rogers, C. A. (1961). On becoming a person. A therapist’s view of psychotherapy. Boston: Houghton and Mifflin Company
- Rogers, A. (1980). A way of being. Boston: Houghton and Mifflin Company.
- Sutanti, N. (2020) 1(2), 47-50 Understanding congruence in person-centred counselling practice: A trainee counsellor’s perspective. Journal of Professionals in Guidance and Counseling, 1(2), 47-50.
- Danvers A et al. (2018). Emotional congruence and judgments of honesty and bias. Collabra: Psychology, 4(1), 1-7.
- Apodaca, C. et al. (2022). Maybe they had a bad day: How LGBTQ and BIPOC patients react to bias in healthcare and struggle to speak out. Journal of the American Medical Informatics Association, 29(12), 2075–2082.
- Boysen, G. (2009). A review of experimental studies of explicit and implicit bias among counselors. Journal of Multicultural Counseling and Development, 37, 240-249.
- Hagiwara, N. et al. (2019). Detecting implicit racial bias in provider communication behaviors to reduce disparities in healthcare: Challenges, solutions, and future directions for provider communication training. Patient Education and Counseling, 102, 1738-1743.
- Crisp, R. (2020). Carl Rogers’ reset with an African American client: a discussion. Person-Centered & Experiential Psychotherapies, 21(3), 220-234.
- 2015). Person and society: towards a person-centered sociotherapy. Person-centered & Experiential Psychotherapies, 14(3), 217-235.
- Kaimaxi, D. & Lakioti, A. (2021). The development of congruence: A thematic analysis of person-centered counselors’ perspectives. Person-centered & Experiential Psychotherapies, 20(3), 232–249.





 Recently, an additional consideration of patients in the LGBTQ community receiving care in these settings indicated comparably positive PDQ results,12 but also raises a question: why wait until the end stage of healthcare? Social dignity violations (e.g., dismissal, disregard, grouping) routinely occur across a wide range of healthcare encounters throughout a lifetime.13-18 There seems no reason to wait: researchers very familiar with the PDQ have pointed out that the PDQ “can be used by any provider type and in numerous care settings to understand patient values” as a standard of care.19 Since all patients seek relational dignity throughout their lives, extending the PDQ intervention to all patients in all settings seems feasible, or at the minimum to those with historical concerns regarding inequitable care.
Recently, an additional consideration of patients in the LGBTQ community receiving care in these settings indicated comparably positive PDQ results,12 but also raises a question: why wait until the end stage of healthcare? Social dignity violations (e.g., dismissal, disregard, grouping) routinely occur across a wide range of healthcare encounters throughout a lifetime.13-18 There seems no reason to wait: researchers very familiar with the PDQ have pointed out that the PDQ “can be used by any provider type and in numerous care settings to understand patient values” as a standard of care.19 Since all patients seek relational dignity throughout their lives, extending the PDQ intervention to all patients in all settings seems feasible, or at the minimum to those with historical concerns regarding inequitable care.
 possesses” (1986, p. 391). More simply, “The factors that influence behavior are embedded in the belief that one has the capability to accomplish that behavior” (Klassen & Klassen, 2018, p. 76).
possesses” (1986, p. 391). More simply, “The factors that influence behavior are embedded in the belief that one has the capability to accomplish that behavior” (Klassen & Klassen, 2018, p. 76).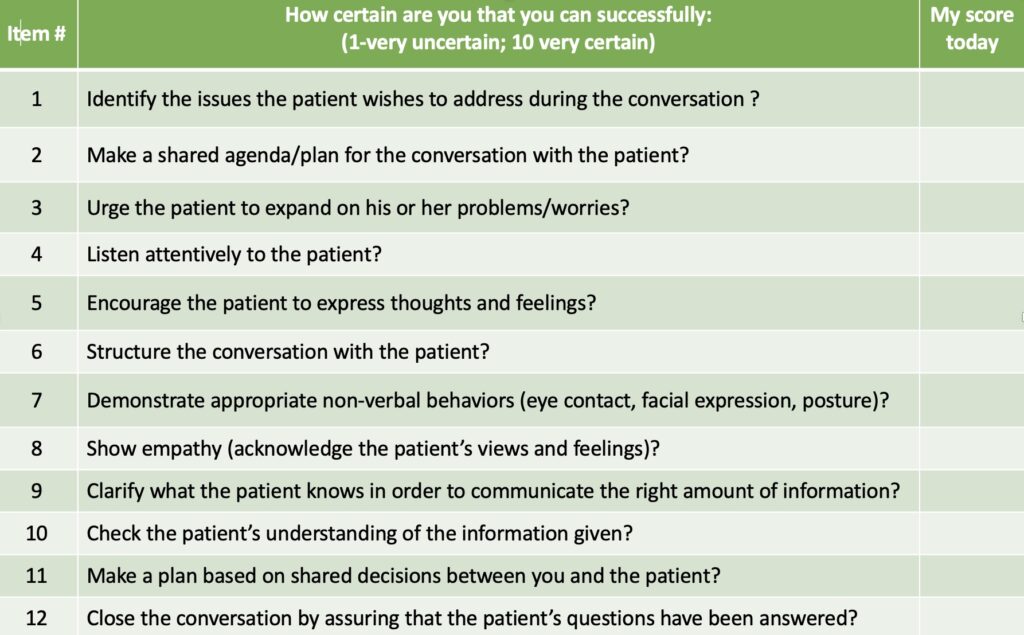


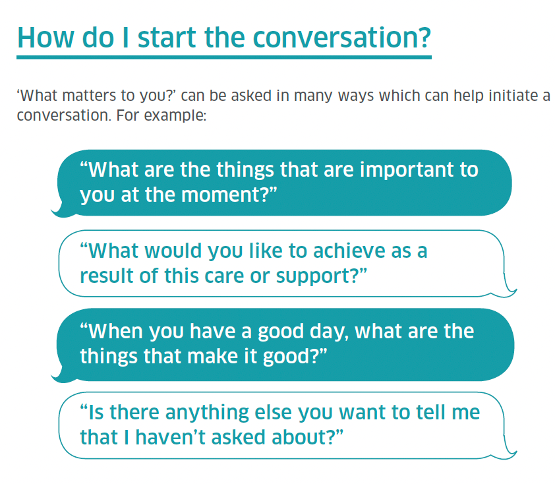

 “Clinician presence” may not be familiar to student trainees, but working with the concept might help them recognize the impact we have on patient impressions and patient outcomes. Clinician presence is defined as a “purposeful practice of awareness, focus, and attention with the intent to understand and connect” (emphasis added) with our patient. Core elements include familiar person/patient-centered behaviors and attributes:2
“Clinician presence” may not be familiar to student trainees, but working with the concept might help them recognize the impact we have on patient impressions and patient outcomes. Clinician presence is defined as a “purposeful practice of awareness, focus, and attention with the intent to understand and connect” (emphasis added) with our patient. Core elements include familiar person/patient-centered behaviors and attributes:2
 patient’s emotions, attitudes, or problems are directly related to living with hearing loss or balance issues; e.g., reactions to diagnosis, concerns about recommendations, or uncertainties about shared decision-making.
patient’s emotions, attitudes, or problems are directly related to living with hearing loss or balance issues; e.g., reactions to diagnosis, concerns about recommendations, or uncertainties about shared decision-making. emotions or behaviors, develops an over-dependence on the clinician, or continues to use offensive language or “overshares”2 after being asked to stop. Clinicians, of course, may also find themselves crossing a boundary, by becoming overly involved with a patient or oversharing about one’s own personal life.
emotions or behaviors, develops an over-dependence on the clinician, or continues to use offensive language or “overshares”2 after being asked to stop. Clinicians, of course, may also find themselves crossing a boundary, by becoming overly involved with a patient or oversharing about one’s own personal life. coordinated healthcare teams. These days, we may likely find ourselves broaching/being broached about topics other than hearing and balance but still relevant to patient health and safety. Audiologists now inquire about medications that may adversely interact with hearing and balance4-7 and are typically required by law to intervene with a referral when we perceive indications of self-harm or suicide ideation.8 Institutions and states require us to report concerns about child and elder abuse.9,10 Other developments include screening for vision problems,11,12 cognitive and memory concerns,13-15 depression,16-19 and childhood bullying20 – of course not to diagnose but to assume responsibility for overall patient health and safety, and direct those concerns to relevant support systems. And although not directly related to our care, of course we will listen and support patients who are coping with a death in the family and similar life experiences. Person-centered care has replaced disease- or disorder-centered care.
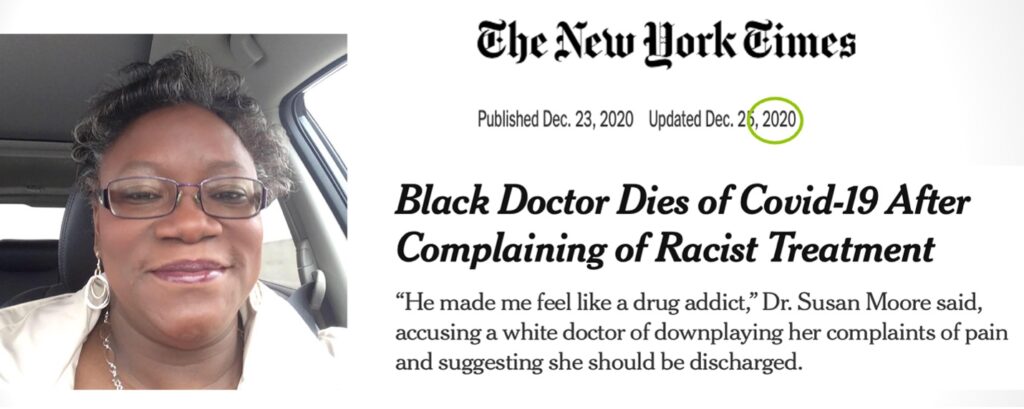
coordinated healthcare teams. These days, we may likely find ourselves broaching/being broached about topics other than hearing and balance but still relevant to patient health and safety. Audiologists now inquire about medications that may adversely interact with hearing and balance4-7 and are typically required by law to intervene with a referral when we perceive indications of self-harm or suicide ideation.8 Institutions and states require us to report concerns about child and elder abuse.9,10 Other developments include screening for vision problems,11,12 cognitive and memory concerns,13-15 depression,16-19 and childhood bullying20 – of course not to diagnose but to assume responsibility for overall patient health and safety, and direct those concerns to relevant support systems. And although not directly related to our care, of course we will listen and support patients who are coping with a death in the family and similar life experiences. Person-centered care has replaced disease- or disorder-centered care. Not surprisingly, within a matter of seconds, racial and ethnic minority patients perceive the “unspoken” and understandably distrust the overall situation, including clinical recommendations.6,7 We cannot ignore how this dynamic undermines our goal of providing racially equitable healthcare – indeed, we are obligated to address the problem.
Not surprisingly, within a matter of seconds, racial and ethnic minority patients perceive the “unspoken” and understandably distrust the overall situation, including clinical recommendations.6,7 We cannot ignore how this dynamic undermines our goal of providing racially equitable healthcare – indeed, we are obligated to address the problem. Time to “Reframe”?
Time to “Reframe”?