
Samantha Tai, PhD
Lecturer | Audiologist
The University of Melbourne
Victoria, Australia
Over the past couple of years, I’ve been asking our new audiology cohort, ‘What characteristics do you think makes a good audiologist?’ Often, there is a pause before a brave hand will come up to say ‘someone who cares about their patient’, another hand will pop up to say ‘someone knowledgeable, who knows a lot about ears’, another calls out ‘someone who is patient and really listens to the patient’, and then another ‘someone who makes the patient feel comfortable’. While the characteristic of being knowledgeable is often highlighted, the thing that baffles me is students’ intuitive recognition that interpersonal skills are a fundamental characteristic of being a good audiologist. Essentially, it comes down to how we make our patients feel.
In recent years, the scope of practice in the audiology profession has expanded from focusing on a site-of-lesion to a holistic, person-centred approach to hearing care (ASHA, 2018; AudA, 2013; BSA, 2016). That is, the role of an audiologist has moved away from simply being a technician who carries out audiological assessments, to a hearing  professional who empowers and supports patients to self-manage their hearing loss. One of the fundamental elements of patient-centred care is the clinician’s ability to respond to patients’ emotions that have stemmed from their hearing loss. Audiologists who display empathy and acknowledge their patient’s emotions can make their patients feel their concerns are validated and help to reduce psychological distress (Ekberg et al., 2014; Poost-Foroosh et al., 2011). The emphasis on investing in the clinician-patient relationship is beginning to gain recognition in the audiologist’s scope of practice around the world. It falls under the professional guidelines as counselling on the psychosocial impact of the hearing loss (ASHA, 2018; AudA, ACAuD and HAASA, 2016; BSA, 2016).
professional who empowers and supports patients to self-manage their hearing loss. One of the fundamental elements of patient-centred care is the clinician’s ability to respond to patients’ emotions that have stemmed from their hearing loss. Audiologists who display empathy and acknowledge their patient’s emotions can make their patients feel their concerns are validated and help to reduce psychological distress (Ekberg et al., 2014; Poost-Foroosh et al., 2011). The emphasis on investing in the clinician-patient relationship is beginning to gain recognition in the audiologist’s scope of practice around the world. It falls under the professional guidelines as counselling on the psychosocial impact of the hearing loss (ASHA, 2018; AudA, ACAuD and HAASA, 2016; BSA, 2016).
Despite the aforementioned benefits, research has found that when our patients do open up and express their underlying concerns, both experienced clinicians and audiology students tend to miss these opportunities to acknowledge our patients’ emotions (Ekberg et al., 2014; Meyer et al., 2017; Tai et al, 2019). This can have a detrimental effect on the clinician-patient relationship and reduce the likelihood of the patient adhering to recommendations (Ekberg et al., 2014; Grenness et al., 2015). We know that limited acknowledgement or empathetic response is not because of a lack of care or preference for patient-centred care, so it raises the question, why does this deficit exist in our clinical practice?
What are the Current Barriers to Responding to Emotions in Audiology?

Can We Use Our Time Differently?
To put it simply, dealing with emotions is hard and several barriers hinder clinicians to adopt these practices in a clinical setting. To understand some of these barriers, we need to first recognize that traditionally, the audiology profession has placed a significant focus on diagnosing and managing the ‘site-of-lesion’. For instance, in a typical audiological appointment, we invest a majority of time assessing the hearing loss and only a limited time to collate all the relevant questions about the patient’s hearing and thoroughly explain the management options. Similarly, when discussing hearing aid options, audiologists are tasked with convincing the patient that hearing devices are beneficial, give a recommendation, perhaps perform an ear impression, and place an order. With the appointment duration set, clinicians and students alike may find themselves adopting a formulaic approach when communicating with patients, and missing opportunities to address patients’ emotional concerns.
In alignment with the audiology culture, the audiology curriculum was developed to foster students’ diagnostic and technical skills in accordance with the scope of practice. Until recently, counselling skills were absent or minimally integrated into the audiology curricula. Consequently, the lack of formal training means that graduates need to learn counselling skills, including how to respond appropriately to patients’ emotional concerns, on the job. Some clinicians are natural communicators with an innate ability to pick up patient cues and respond empathetically. Honestly, I wouldn’t classify myself as a natural communicator and perhaps there are those of you out there who can relate. I’m sure there are clinicians out there who do not feel comfortable addressing our patient’s emotions because there is
an underlying fear that we might make them feel worse. Without further upskilling or training in counselling skills, experienced clinicians may be unaware of the benefits of acknowledging patient emotions, resulting in the provision of suboptimal hearing care to patients. And through no fault of their own, the missed opportunities to invest in the client-patient relationship may be observed by new graduates or students on clinical placements, who will miss a valuable lesson on how to build a therapeutic relationship.
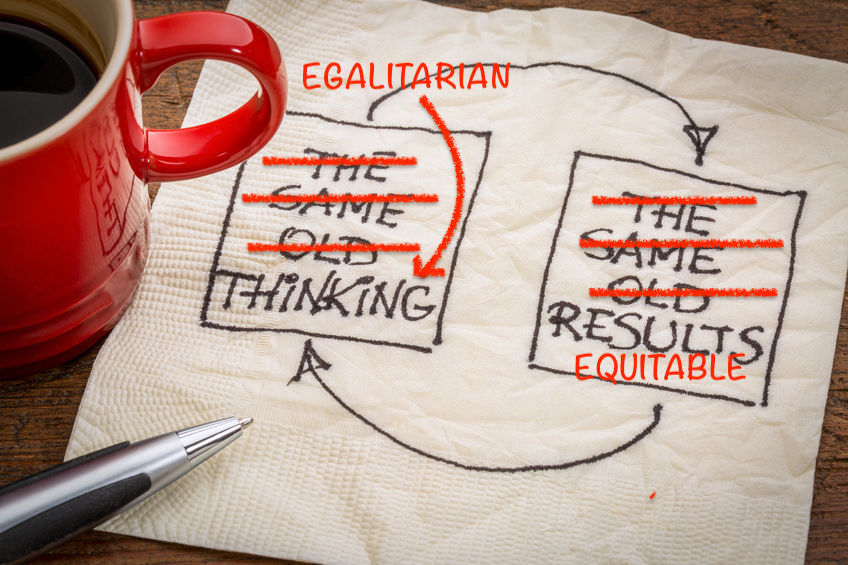
So What Can We Do to Improve This?
As audiologists, we carry the responsibility to do what’s right by our patients. Although there are things we can’t control such as our educational past or the culture of our workplace, there are plenty of things that are within our control.
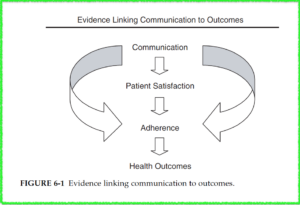
Firstly, we need to recognize the way we interact with our patients carries a significant effect on our patient’s hearing outcome. This includes whether they understand their hearing loss, to whether they take your advice about getting an MRI to investigate their asymmetrical hearing loss, or getting and wearing their hearing devices. When we tell our patients they have a hearing loss, we often forget that we’re delivering bad news. On the surface, our patients may be putting on a brave face as they try to listen intently as we describe the circles and crosses on the graph (FYI, sometimes it’s best not to show patients the audiogram). We lose sight that our patients are trying to decipher how their hearing loss will impact their relationships, hobbies, work and perhaps their self-image. If we understand the emotional toll our patients are experiencing due to their hearing loss, then we are more inclined to try and support them through it.
Secondly, we need to critically and honestly examine our own clinical practice and identify any areas that need improvement. In this piece, we’ve focused on acknowledging patient emotions, but it also extends to other areas in our practice. One method is the use of  self-reflective practice where we take a couple of minutes after each appointment to reflect on what went well and what can be improved. Bringing the focus back to addressing patient emotions, we may find that when we recognize and acknowledge our patient’s emotional concerns, he/she starts opening up and we have developed a better rapport. Conversely, we may have noticed a missed opportunity when our patient seemingly joked about early retirement because he can’t carry out his normal work duties. Both scenarios are wonderful opportunities for professional growth and life-long learning.
self-reflective practice where we take a couple of minutes after each appointment to reflect on what went well and what can be improved. Bringing the focus back to addressing patient emotions, we may find that when we recognize and acknowledge our patient’s emotional concerns, he/she starts opening up and we have developed a better rapport. Conversely, we may have noticed a missed opportunity when our patient seemingly joked about early retirement because he can’t carry out his normal work duties. Both scenarios are wonderful opportunities for professional growth and life-long learning.
Finally, we need to invest in ourselves to improve the deficits in our clinical practice. There are many established teaching frameworks available that outlines the key elements of patient-centred communication. For instance, the Calgary Cambridge Guides (Kurtz et al., 1996), or the Four Habits (Krupat et al, 2006) are examples of evidence-based frameworks in medicine that can be translated to an audiological setting. There are also free training resources from the Ida Institute that provides counselling tools for experienced clinicians and students. If other work colleagues are interested in some upskilling, in-house case discussions can include communication strategies to counsel patients in different scenarios. There may even be opportunities for peer learning by observing your colleague’s appointment. Be creative!

References
American Speech-Language-Hearing Association. (2018). Scope of Practice in Audiology. [Accessed October 18, 2018]
AudA, ACAud, & HAASA. (2016). Scope of Practice for Audiologists and Audiometrists, (September), 1-23. [Accessed October 18, 2018]
Audiology Australia. (2013). Professional Practice Standards – Part A Clinical Operations. [Accessed March 29, 2016]
British Society of Audiology. (2016). Practice Guidance: Common Principles of Rehabilitation for Adults in Audiology Services. [Accessed January 17, 2017]
Ekberg, K., Grenness, C., & Hickson, L. (2014). Addressing patients’ psychosocial concerns regarding hearing aids within audiology appointments for older adults. American Journal of Audiology, 23(3), 337–350.
Grenness, C., Hickson, L., Laplante-Lévesque, A., Meyer, C., & Davidson, B. (2015). Communication patterns in audiologic rehabilitation history-taking: Audiologists, patients, and their companions. Ear and Hearing, 36(2), 191–204.
Krupat, E., Frankel, R., Stein, T., & Irish, J. (2006). The Four Habits Coding Scheme: Validation of an instrument to assess clinicians’ communication behavior. Patient Education and Counseling, 62(1), 38-45.
Kurtz, S. M., & Silverman, J. D. (1996). The Calgary-Cambridge Referenced Observation Guides: an aid to defining the curriculum and organizing the teaching in communication training programmes. Medical Education, 30(2), 83–89.
Meyer, C., Barr, C., Khan, A., & Hickson, L. (2017). Audiologist-patient communication profiles in hearing rehabilitation appointments. Patient Education and Counseling, 100(8), 1490–1498.
Poost-Foroosh, L., Jennings, M. B., Shaw, L., Meston, C. N., & Cheesman, M. F. (2011). Factors in client-clinician interaction that influence hearing aid adoption. Trends in Amplification, 15(3), 127–139.
Tai, S., Barr, C., & Woodward-Kron, R. (2019). Towards patient-centred communication: An observational study of supervised audiology student-patient hearing assessments. International Journal of Audiology, 58(2), 97-106.
 Kris English, PhD
Kris English, PhD







 professional who empowers and supports patients to self-manage their hearing loss. One of the fundamental elements of patient-centred care is the clinician’s ability to respond to patients’ emotions that have stemmed from their hearing loss. Audiologists who display empathy and acknowledge their patient’s emotions can make their patients feel their concerns are validated and help to reduce psychological distress (Ekberg et al., 2014; Poost-Foroosh et al., 2011). The emphasis on investing in the clinician-patient relationship is beginning to gain recognition in the audiologist’s scope of practice around the world. It falls under the professional guidelines as counselling on the psychosocial impact of the hearing loss (ASHA, 2018; AudA, ACAuD and HAASA, 2016; BSA, 2016).
professional who empowers and supports patients to self-manage their hearing loss. One of the fundamental elements of patient-centred care is the clinician’s ability to respond to patients’ emotions that have stemmed from their hearing loss. Audiologists who display empathy and acknowledge their patient’s emotions can make their patients feel their concerns are validated and help to reduce psychological distress (Ekberg et al., 2014; Poost-Foroosh et al., 2011). The emphasis on investing in the clinician-patient relationship is beginning to gain recognition in the audiologist’s scope of practice around the world. It falls under the professional guidelines as counselling on the psychosocial impact of the hearing loss (ASHA, 2018; AudA, ACAuD and HAASA, 2016; BSA, 2016).
 self-reflective practice where we take a couple of minutes after each appointment to reflect on what went well and what can be improved. Bringing the focus back to addressing patient emotions, we may find that when we recognize and acknowledge our patient’s emotional concerns, he/she starts opening up and we have developed a better rapport. Conversely, we may have noticed a missed opportunity when our patient seemingly joked about early retirement because he can’t carry out his normal work duties. Both scenarios are wonderful opportunities for professional growth and life-long learning.
self-reflective practice where we take a couple of minutes after each appointment to reflect on what went well and what can be improved. Bringing the focus back to addressing patient emotions, we may find that when we recognize and acknowledge our patient’s emotional concerns, he/she starts opening up and we have developed a better rapport. Conversely, we may have noticed a missed opportunity when our patient seemingly joked about early retirement because he can’t carry out his normal work duties. Both scenarios are wonderful opportunities for professional growth and life-long learning.



 A close reading of our ethics texts leads us to appreciate the ethical implications of listening (or not listening) to our patients. If we don’t fully absorb patient narratives, we are less likely to be “moved to action” toward personalized and comprehensive care. Promoting “close listening” (in the context of PCC) as an ethical practice warrants review and discussion within the profession.
A close reading of our ethics texts leads us to appreciate the ethical implications of listening (or not listening) to our patients. If we don’t fully absorb patient narratives, we are less likely to be “moved to action” toward personalized and comprehensive care. Promoting “close listening” (in the context of PCC) as an ethical practice warrants review and discussion within the profession. Kris English, PhD
Kris English, PhD To manage the potential conflict between maintaining patient relationships and electronic records, let’s consider a relatively simple communication skill called signposting. The following definitions of signposting will resonate, since they are already routine practices in audiologic practice:
To manage the potential conflict between maintaining patient relationships and electronic records, let’s consider a relatively simple communication skill called signposting. The following definitions of signposting will resonate, since they are already routine practices in audiologic practice:
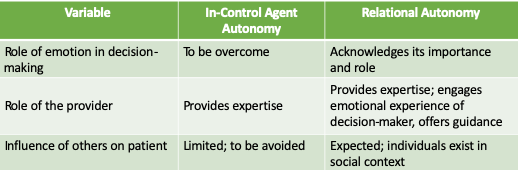
 This template assumes the clinician welcomes and supports SDM. Unfortunately, our available evidence suggests this assumption is not a given (e.g., Ekberg et al, 2015; Grenness et al., 2015). Our limited research has also only focused on decisions related to hearing aid acceptance and options. However, there are other SDM opportunities in an audiology appointment, and these could be easily overlooked.
This template assumes the clinician welcomes and supports SDM. Unfortunately, our available evidence suggests this assumption is not a given (e.g., Ekberg et al, 2015; Grenness et al., 2015). Our limited research has also only focused on decisions related to hearing aid acceptance and options. However, there are other SDM opportunities in an audiology appointment, and these could be easily overlooked. A student exercise: How do these comments differ? How might a patient respond/react to each, and why? What counseling/communication skills do you recognize? These essays provide some relevant background:
A student exercise: How do these comments differ? How might a patient respond/react to each, and why? What counseling/communication skills do you recognize? These essays provide some relevant background: